30 years old female with Fever and B/L knee pain
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box.
E.Siddhanth 157
A 31year old female, who studied till degree and is a housewife by occupation came with chief complaints of:
B/L knee pains since 2 weeks
Fever on and off since 2 weeks
Oral ulcers since 6 months
Patient was apparently asymptomatic 2 years ago and then she developed pain in her right shoulder, which was dull aching type and continuous, for which she went to an Orthopaedic and was given medication. The pain kept alternating between right and left shoulder and sometimes both simultaneously. She experienced tightness of shoulder joints on waking up and needs someone to pull her up from the bed. Her pain was relieved on medication but it kept recurring for 6 months.
After 1 month of developing shoulder pain,her proximal interphalangeal joints were swollen, which was associated with decreased function as she was not able to write properly, open bottle cap etc.
She also developed B/L knee pains and generalized weakness.
Then she developed fever, oral ulcers ( was not able to eat food) , redness of eyes and diminished vision, facial puffiness and went to a private hospital.
She also developed hair loss 2 years ago, which was gradually progressive.
On routine investigations, they found that she was losing a lot of proteins ( nephrotic range proteinuria) in her urine, and increased protein creatinine ratio of 4.99, due to which and her diminishing vision they decided to a kidney biopsy.
Renal biopsy was done on 5/08/2022
Biposy showed focal mild increased endocapillary cellularity pointing towards FOCAL GLOMERULONEPHRITIS, after which the diagnosis of SLE was made as she also showed positive ANA profile as follows:
Anti -RNP/ Sm and Anti- Sm, Anti-Jo 1, Anti - ds DNA, nucleosomes and RIBOSOMAL P- PROTEIN
She was put on Tab. OMNOCORTIL 50 mg for 3 days and steroid injections and was tapered over 6 months to 2.5mg.
After 6 months, steroids were stopped and was started on
Tab. MFM for 4 months (2 tab at 8 AM and 1 tab at 8 PM), which she used and stopped after one month after tapering. She was also advised to perform exercises.
IN FEBRUARY 2021, She was started on FOLITRAX after which she noticed increase in number of oral ulcers , so she went to a private hospital 15 days later, and was started again started on OMNOCORTIL 5mg
She later developed blurring of vision more in day light, for which she was diagnosed with cataract in her left eye
Past history:
Treatment history:
Patient is currently on:
Tab. MMF 500mg PO BD (8AM & 8 PM)
Tab. FOLITRAX 10mg weekly once
Tab. LIVOGEN PO BD
TAB. HCQ 200mg OD
Tab. SHELCAL PO OD
Tab. THYRONORM 50mcg
General examination:
Patient is conscious, coherent and cooperative.
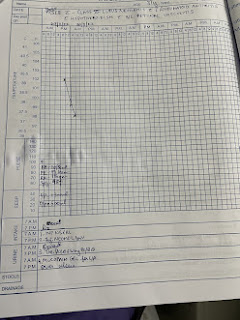
Vitals on admission:
Temp: 102°F
BP: 120/80
PR: 110 bpm
CVS: S1 S2 present N
o murmurs or thrills heard
RS: BAE present, NVBS heard
CNS: E4V5M6
P/A: soft, non tender










Comments
Post a Comment